SURGICAL ISSUES
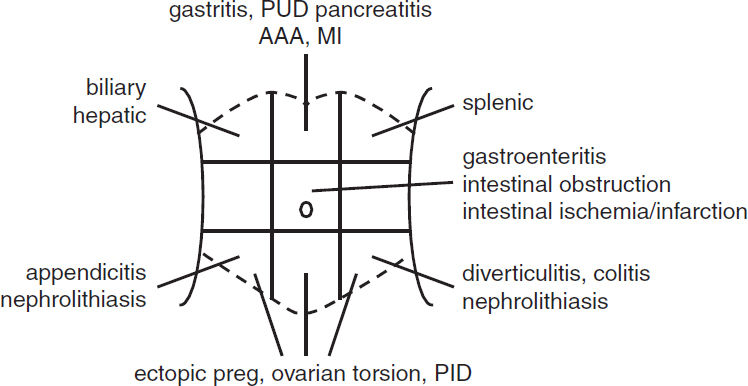
ABDOMINAL PAIN
Visceral Pain |
||
Anatomic Division |
Viscera |
Area to Which Pain Referred |
Foregut |
Esophagus & duodenum |
Epigastrium |
Midgut |
Jejunum to mid-transverse colon |
Umbilicus |
Hindgut |
Mid-transverse colon to rectum |
Hypogastrium |
Pain due to pancreatitis and nephrolithiasis commonly radiates to the back
Initial evaluation
• History: onset of pain, location, exacerbating/relieving factors
• Assoc. sx: fevers/chills, N/V, Δ in bowel habits (diarrhea/constipation, stool diam. or color, hematochezia, melena), flatus, jaundice, Δ in urine color, Δ in wt, menstrual hx in women
• PMHx: previous incisions or abdominal surgeries; Ob/Gyn hx
• Exam: VS; general posture of Pt; comprehensive abdominal exam looking for signs of peritonitis, which include rebound tenderness and involuntary guarding, abdominal wall rigidity, pain w/ percussion/minimal palpation; presence of hernias; rectal/pelvic
• Labs: CBC, electrolytes, LFTs, amylase/lipase, pregnancy test
• Imaging: depends on suspected etiology, may include RUQ U/S for biliary/hepatic disease, KUB for intestinal obstruction, CT for pancreatitis or intestinal disease. Do not delay resuscitation or surgical consultation for ill Pt while waiting for imaging.
ACUTE ABDOMEN
Definition
• Acute onset abdominal pain that portends need for urgent surgery
Etiologies
• Perforated viscus → peritonitis (perforated ulcer, complicated diverticulitis, trauma)
• Intraperitoneal or retroperitoneal bleed (also see “Acute Aortic Syndromes”)
• Bowel obstruction (adhesions from previous surgeries, malignancies, hernias, volvulus)
• Acute mesenteric ischemia (esp. if AF, low flow states, “pain out of proportion to exam”)
• Mimics: severe pancreatitis can resemble peritonitis; renal colic causes severe abdominal pain but not abdominal rigidity
Initial evaluation
• H&P as above
• Labs as above plus: PT/INR, PTT, lactate, type & screen (crossmatch if active bleeding)
• Imaging: upright CXR/KUB; if stable, CT A/P w/ IV contrast (IV/PO if suspect obstruction)
Initial management
• Immediate surgical consultation for suspected acute abdomen
• NPO, start IV fluids (NS or LR), Foley, NGT placement if obstruction suspected
• Broad spectrum abx if perforation suspected
EXTREMITY EMERGENCIES
Acute limb ischemia (see “Peripheral Artery Disease” for details)
• Definition: sudden ↓ in perfusion causing threat to limb viability
• Eval: detailed vascular exam (incl. pulses & Doppler signals, motor/sensory function); CTA
• Initial management: anticoag for embolism/thrombosis (heparin dose 80 U/kg bolus, then 18 U/kg drip); immediate surgical consultation
Compartment syndrome (Clin Orthop Relat Res 2010;468:940)
• Definition: ↑ intracompartmental pressure w/ compressive closure of venules → ↑ hydrostatic force resulting in further increases in compartment pressure
• Etiologies: orthopedic (fracture), vascular (ischemia-reperfusion), iatrogenic (eg, vascular injury in anticoagulated Pt), soft-tissue injury (eg, prolonged limb compression)
• Clinical manifestations: pain espec. on passive movement, swollen/tense compartment, paraesthesia, pallor, pulselessness, paralysis (late)
• Evaluation: surgical evaluation of compartment pressures; intracompartment pressure >30 or difference between diastolic & intracompartment pressure of >10–30 is diagnostic
• Treatment: fasciotomy
SURGICAL TUBES, DRAINS, WOUNDS
Tracheostomy (Otolaryngol Head Neck Surg 2013;148:6)
• Typically a cuffed tube, which creates a tight seal to facilitate ventilation throughout tube
• Speaking valve (eg, Passy-Muir): 1-way valve that allows inhalation through tube, but exhalation around tube through vocal cords (nb, cuff should not be inflated)
• 1st routine tube Δ for percutaneously placed tubes should be ~10 d postop; surgically placed tubes can be Δ’d >5 d postop; first Δ should be overseen by experienced person
• Accidental dislodgement: intubate from above (if airway/vent nec & anatomically possible)
w/in 7 d of placement: emergent surgical consultation
>7 d after placement: replace with a similar size tube or smaller
Chest tubes (Eur J Cardiothorac Surg 2011;40:291)
• Inserted for PTX, chest trauma or after thoracic surg for drainage of air/fluid from thoracic cavity. Range from small (8–10 Fr for spont. PTX) to large (28–32 Fr after pulm. resections)
• Connected to 3-chamber chest drainage system:
1st: collection chamber for pleural fluid
2nd: water seal chamber used to allow air to exit pleural space on exhalation and prevent air from entering on inhalation
3rd: suction control chamber which regulates suction transmitted to pleural space
• Monitor for output and presence of air leak (indicated by bubbling in water seal chamber)
• Removal determined by overall daily outputs and absence of air leak
• If accidentally removed or dislodged, tube should be completely removed and an occlusive dressing (eg, 4 × 4 covered w/ Tegaderm or silk tape) should be placed rapidly over site. CXR STAT; new tube should be placed if persistent PTX.
Gastrostomy/jejunostomy tubes (Paediatr Child Health 2011;16:281)
• Placed for tube feedings, hydration, and delivery of medications
• Should not be removed for ≥6–8 wk to allow establishment of mature gastrocutaneous tract
• Obstructed tubes can be cleared by flushing with agents such as carbonated water, meat tenderizer, & pancreatic enzymes. ↓ obstruction by flushing before & after meds and flushing q4–6h when receiving continuous feeds.
• Inadvertent removal: place Foley catheter of similar size or smaller into tract immediately to prevent stoma from closing. Tube then replaced and confirmed via fluoro study.
Suture/staple removal
• Should be done in consultation w/ surgical team; timing depends on location of wound
• Should not be removed if there is evidence of wound separation during removal!
• After removal, wound should be reapproximated w/ Steri-Strips
Decubitus ulcers (J Wound Ostomy Continence Nurs 2012;39:3)
• Sores in dependent areas exposed to repeated pressure (commonly sacrum, heels)
• Risk factors: immobility, poor nutritional status
• Stage I (non-blanchable erythema); Stage II (partial thickness); Stage III (full-thickness skin loss); Stage IV (full-thickness tissue loss)
• Treatment: offload area, air mattress, pillows and/or support boots, nutritional support
• Surgical consultation for debridement of ulcers with necrotic or infected tissue, may require plastic surgical reconstruction for advanced ulcers once clean
MAXIMIZING A SURGICAL CONSULT
• For ill Pt, call surgical consult early, do not wait for labs & imaging results
• If potential surgical emergency, make Pt NPO, start IVF, ✓ coags, type, & screen
• Have appropriate-level MD who knows & has examined Pt call consult
OB/GYN ISSUES
VAGINAL BLEEDING
Bleeding from lower (vulva, vagina, cervix) or upper genital tract (uterus)
Etiologies
• Premenopausal
Not pregnant: menses, lower tract (trauma, STI, cervical dysplasia/cancer), & abnormal uterine bleeding (polyp, adenomyosis, leiomyoma, hyperplasia/cancer, coagulopathy, ovulatory dysfunction, endometrial, & iatrogenic)
Pregnant
1st trimester: threatened abortion, spont. abortion (missed, incomplete, or complete), ectopic preg, molar preg (partial/complete hydatidiform mole)
2nd or 3rd trimester: preterm labor/labor, placenta previa, placental abruption
• Postmenopausal: atrophy, polyp, leiomyoma, endometrial hyperplasia/cancer
History & exam
• Age, menopausal status, gestational age if preg, volume & duration of current bleeding
• If premenopausal: menstrual hx including age of onset, interval between & duration of menses, any assoc. sx & LMP to assess timing of menstrual cycle
• Past Ob/Gyn hx: incl. any structural abnl, STI, & contraception
• Health maint.: Pap smear, HPV screening, domestic violence, anticoag/antiplt meds
• General physical & abdominal exam (incl. tenderness, masses)
• Pelvic exam: external (quantity of bleeding seen on vulva, any lesions, any trauma), speculum exam (quantity of bleeding, cervical os open/close; & if open, dilation, any polyps), & bimanual exam (cervical dilation, uterine size/tenderness, adnexal mass/tenderness)
Laboratory evaluation & imaging
• Urine (rapid test) & serum preg test (βhCG), Hct/hemoglobin
• Pelvic U/S: visualize leiomyoma & if preg, intrauterine preg & placental position to r/o placenta previa/abruption
• If preg & intrauterine preg not seen, must r/o ectopic as life-threatening dx (βHCG > discrim. zone → ? ectopic; if βHCG <discrim. zone → follow βHCG) (JAMA 2013;309:1722)
VAGINAL DISCHARGE
Fluid or mucus from vagina, cervix, or uterus
Etiologies
• Infectious: bacterial vaginosis, candida vulvovaginitis, trichomoniasis
• Noninfectious: physiologic (in preg/non-preg), rupture of membranes, foreign-body rxn
Initial evaluation
• Age, LMP, gestational age if preg or menopausal status
• Discharge quantity, color, consistency, odor, assoc. sx (itchiness, redness, abd/pelvic pain)
• Past Gyn hx: incl. STI and contraception usage (condoms ↓ STI risk)
• Tampon or condom use as risk factors for retained foreign body
• Pelvic exam: external (quantity & quality of discharge on vulva, any lesions), speculum (discharge, appearance of cervix), bimanual (cervical motion tenderness)
• Laboratory: pH of discharge, microscopy (saline & KOH wet mounts), urine preg test
Treatment
• Bacterial vaginosis: oral/vaginal metronidazole or clindamycin
• Candida vulvovaginitis: oral/topical antimycotic medications
• Trichomoniasis: oral metronidazole
ADNEXAL MASS IN NON-PREGNANT WOMAN
Mass arising from ovary, fallopian tube, or surrounding connective tissue
Etiologies
• Ovarian: functional cyst (follicular/corpus luteum), hemorrhagic cyst, endometriomas, ovarian torsion, tubo-ovarian abscess, benign & malignant ovarian tumors
• Fallopian tube: paratubal cyst, hydrosalpinx, ovarian torsion, tubo-ovarian abscess
Initial evaluation
• LMP/menopausal status, assoc. sx of abd/pelvic pain, FHx of gyn cancers
• Abd exam (distension, tenderness, masses), bimanual (uterine or adnexal masses)
• Preg test if premenopausal (if ⊕, then mass likely preg), CA-125 if postmenopausal
• Pelvic U/S (even if mass 1st identified on CT, because U/S is best modality), U/S appearance of mass important factor to determine risk of malignancy
OPHTHALMIC ISSUES
INITIAL EVALUATION
• Ocular symptom: onset (sudden or progressive) & duration of sx; unilateral vs. bilateral; pain; photophobia; discharge; Δ in near (eg, book) or far (eg, TV across room) vision
• Preexisting ocular conditions, eye meds (incl any Δs), recent h/o ocular surgery, trauma
• Ocular exam: vision (✓ with Pt’s correction [glasses/contacts]) w/ each eye; pupillary exam; EOM; confrontation visual fields (important if suspect CNS problem)
• Overall: VS, immunocomp., s/s of infxn, h/o malig, CNS issues, Δ in meds, CBC, coags
COMMON VISUAL SYMPTOMS
• Fluctuation in vision (ie, blurry): med-induced refractive error (eg, systemic steroids, chemoRx), hyperglycemia, dry eye (common). Visual defect may p/w “blurred vision.” Bilateral: glaucoma (common), homonymous contral. CNS lesion; bitemporal: pituitary, toxic/nutritional. Unilateral: ipsilateral orbital, retinal, or optic nerve lesion.
• Red eye:
Bilateral: viral conjunct. (starts in 1 eye; also w/ lid swelling, discharge); chronic inflammation (dry eyes, rosacea, autoimmune disease)
Unilateral: subconj. hemorrhage, infxn, or inflam (eg, episcleritis, iritis, uveitis, scleritis); acute angle closure (qv). Scleritis & acute angle closure p/w severe pain, H/A, nausea.
• Double vision (diplopia): fixed double vision w/ ophthalmoplegia from orbital process or cranial nerve palsy (III, IV, VI). Transient “diplopia” due to fatigue or sedation.
• Flashing lights/floaters: vitreous detach. (common, benign); retinal detach. (unilateral visual field defect; urgent ophthalmology consult); hemorrhage; intraocular lymphoma
ACUTE VISUAL CHANGES
Etiologies of Acute Vision Loss (italics indicates a/w pain) |
||
|
Unilateral |
Bilateral |
Transient (<24 h, often <1 h) |
Ret. art. embolism, impending retinal artery or vein occlusion (amaurosis fugax), vasospasm, carotid disease |
Ocular surface dis. (dry eye), bilat. carotid dis., TIA, migraine, high ICP (papilledema) |
Prolonged (>24 h) |
Retinal art/vein occl, retinal detach., retina/vitreous heme, retinitis, ant. optic neurop./corneal ulcer, GCA, acute angle closure glaucoma |
Visual cortex stroke, post. ischemic neuropathy (profound hypotension during surgery), post. reversible enceph. synd., GCA |
COMMON OCULAR CONDITIONS (FRONT TO BACK)
• Orbit: orbital cellulitis (fever, proptosis, ↓ EOM; emergent abx, scan, & referral)
• Lids: hordeolum or chalazion (stye); preseptal cellulitis; ptosis (age; Horner’s; CN III palsy: EOM restricted in all directions except laterally (eye is “down & out”), a/w ptosis & mydriasis, seen w/ uncal herniation, aneurysm of post com art., GCA, HTN, DM); incomplete lid closure (CN 7th palsy)
• Conjunctiva: conjunctivitis (red eye); subconj. hemorrhage (HTN, blood thinner); ocular surface disease (dry eyes); episcleritis/scleritis (deep vessels of sclera)
• Cornea: contact lens-related ulcer; herpetic keratitis/scarring/neurotropic ulcers (CN V paresis); pterygium; keratoconus; corneal dystrophy
• Ant. chamber: iritis (inflam. cells); hyphema (blood, post trauma); hypopyon (inflam./infxn)
• Pupil: Anisocoria (physiologic asymmetry); Horner’s, CN III
• Lens: cataract (age, trauma, medication, radiation, congenital); post cataract surgery infxn
• Vitreous/Retina/Macula: diabetic retinopathy; macular degen; retinal detachment; retinal ± vitreous hemorrhage; retinitis (infectious)
• Optic nerve (CN II): ischemic neuropathy p/w acute unilat. visual loss, altitudinal field defect; a/w GCA; nonarteritic a/w HTN, hyperchol., DM, thrombophilia. Optic neuritis: often p/w unilat. central scotoma, pain w/ EOM, ↑ visual loss over days; a/w demyelinating disease (eg, MS), also seen w/ sarcoidosis & CTD. Optic neuropathy (glaucoma common).
OCULAR EMERGENCIES
• Chemical splash: alkali worse than acid; immediate eye flush; pH 7.3–7.4 normal
• Acute angle closure glaucoma: fixed mid-dilated pupil, corneal edema, high intraocular pressure (typically >50; normal 8–21). Rx w/ topical drops; may require AC tap/laser.
• Penetrating eye injury: protect eye (no patching), IV abx, tetanus, NPO, surgical prep
Table of contents
- Cover
- Title Page
- Copyright Page
- Contents
- Contributing Authors
- Foreword
- Preface
-
CARDIOLOGY
- Electrocardiography
- Chest Pain
- Noninvasive Evaluation of CAD
- Coronary Angiography & PCI
- Stable Ischemic Heart Disease
- Acute Coronary Syndromes
- PA Catheter and Tailored Therapy
- Heart Failure
- Cardiomyopathies
- Valvular Heart Disease
- Pericardial Disease
- Hypertension
- Aortic Aneurysms
- Acute Aortic Syndromes
- Arrhythmias
- Atrial Fibrillation
- Syncope
- Cardiac Rhythm Management Devices
- Cardiac Risk Assessment for Noncardiac Surgery
- Peripheral Artery Disease
-
PULMONARY
- Dyspnea
- Pulmonary Function Tests
- Asthma
- Anaphylaxis
- Chronic Obstructive Pulmonary Disease
- Solitary Pulmonary Nodule
- Hemoptysis
- Bronchiectasis
- Cystic Fibrosis
- Interstitial Lung Disease
- Pleural Effusion
- Venous Thromboembolism
- Pulmonary Hypertension
- Respiratory Failure
- Mechanical Ventilation
- Acute Respiratory Distress Syndrome
- Sepsis and Shock
- Toxicology
- Lung Transplant
- GASTROENTEROLOGY
- NEPHROLOGY
-
HEMATOLOGY-ONCOLOGY
- Anemia
- Disorders of Hemostasis
- Platelet Disorders
- Coagulopathies
- Hypercoagulable States
- Disorders of Leukocytes
- Transfusion Therapy
- Myelodysplastic Syndromes
- Myeloproliferative Neoplasms
- Leukemia
- Lymphoma and CLL
- Plasma Cell Dyscrasias
- Hematopoietic Stem Cell Transplantation
- Lung Cancer
- Breast Cancer
- Prostate Cancer
- Colorectal Cancer
- Pancreatic Tumors
- Other Solid Tumors
- Immunotherapy & Cellular Therapy
- Oncologic Emergencies
- Chemo Side Effects
- INFECTIOUS DISEASES
- ENDOCRINOLOGY
-
RHEUMATOLOGY
- Approach to Rheumatic Disease
- Rheumatoid Arthritis
- Adult-Onset Still’s Disease & Relapsing Polychondritis
- Crystal Deposition Arthritides
- Seronegative Spondyloarthritis
- Infectious Arthritis & Bursitis
- Connective Tissue Diseases
- Systemic Lupus Erythematosus
- IgG4-Related Disease
- Vasculitis
- Autoinflammatory Syndromes
- Amyloidosis
- NEUROLOGY
- CONSULTS
- APPENDIX
- ABBREVIATIONS
- INDEX
- PHOTO INSERTS
- ACLS